DICON faculty and SSI expert Dr. Jessie Seidelman and DICON Medical Director D. Dev Anderson provided an update on SSIs to the journal Infection Disease Clinics of North America.
Surgical site infections (SSIs) are among the most common and most costly health care–associated infections, leading to adverse patient outcomes and death. Wound contamination occurs with each incision, but proven strategies exist to decrease the risk of SSI. In particular, improved adherence to evidence-based preventive measures related to appropriate antimicrobial prophylaxis can decrease the rate of SSI. Aggressive surgical debridement and effective antimicrobial therapy are needed to optimize the treatment of SSI.
-
Surgical site infections (SSIs) are associated with prolonged hospitalizations, death, and overall poor patient outcomes.
-
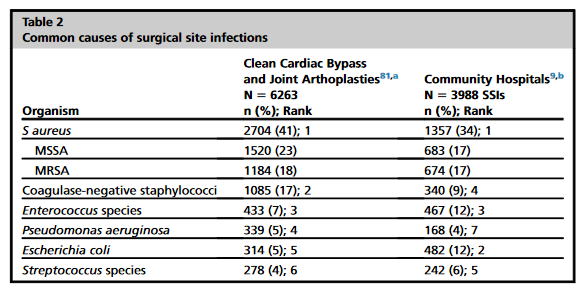
SSIs are typically caused by pathogens inoculated at the time of surgery from the patient’s own flora.
-
SSI acquisition depends on exposure to bacteria and the host’s ability to control the inevitable bacterial contamination of the surgical wound.
-
The 9 core best practices to reduce SSIs address preoperative bathing, antimicrobial prophylaxis, preoperative surgical site preparation, surgical hand preparation, normothermia, hyperoxygenation, wound protectors, glucose control, and perioperative checklist.
-
SSI surveillance and feedback decrease SSI rates and are recommended by Centers for Disease Control and Prevention.
SSIs are the most common and costly health care–associated infections in the United States and lead to significant patient morbidity and mortality. However, adhering to evidence-based preventive practices can decrease the rate of SSI. In general, aggressive surgical debridement in addition to appropriate antibiotic therapy is necessary for SSI treatment.
